It’s a Virtual World: Harnessing Technology to Enhance Type 1 Diabetes Care
No one is untouched by COVID-19, but there are unique and severe risks for those living with Type 1 diabetes.
Type 1 diabetes is an autoimmune disease where the immune system destroys the cells that make insulin, a hormone required to maintain tight control of blood sugar (glucose) levels in the body. Blood sugar levels that drop too low lead to confusion, loss of consciousness and even death. Blood sugar levels that are too high lead to nausea, fatigue and over the long term, organ damage.1,2
Virtual Management of Diabetes During COVID-19
Given the severe consequences of Type 1 diabetes, close management of the disease is essential. Yet, frequent healthcare visits put those with Type 1 diabetes at higher risk of exposure to COVID-19.
And if someone with Type 1 diabetes contracts COVID-19? Research suggests that individuals with diabetes experience more severe symptoms and are more likely to be hospitalized from COVID-19 than someone without diabetes.1
Virtual care may be the only option to minimize exposure to the virus while maintaining close management of the disease.
Dr. Angelo Simone, an endocrinologist at Mississauga Hospital, believes “the COVID-19 outbreak could have long-lasting impacts on how people with diabetes access care, as virtual appointments could become the norm.”
New technologies that allow patients and doctors the ability to access blood sugar data virtually are game changers. “Technologies like integrated sensors that transmit data to clinics are providing the information used for virtual care,” explains Dr. Simone. “We can look at the data together and make informed decisions that guide better insulin management.”
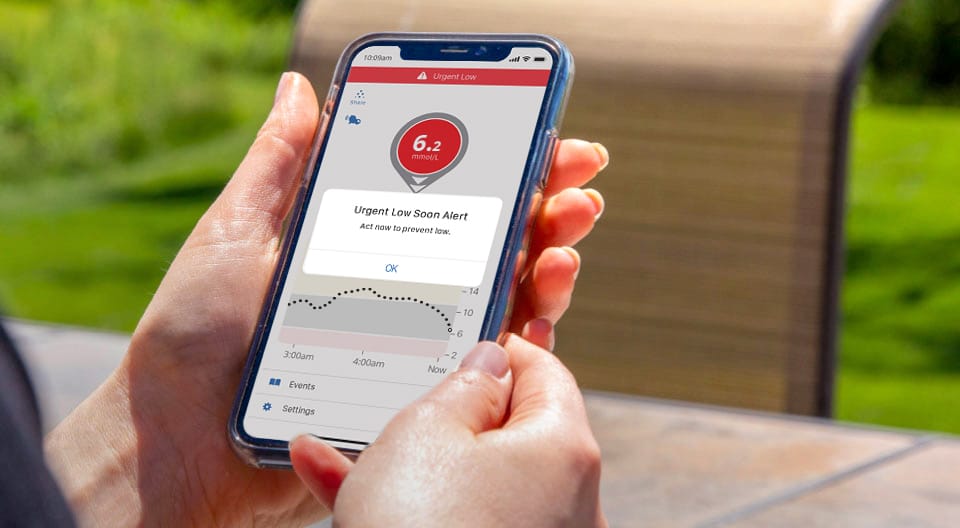
Integrated sensor technology like Continuous Glucose Monitoring measures blood sugar levels in real-time and can send that data back to the individual, their family and their physician.
The sensor sends an alarm to the individual and their support network when values are out of range so that insulin levels can be modified quickly.
Dr. Simone notes that these devices eliminate the need for “frequent finger pricks to test blood glucose, and reduce worries overnight, as there is an alarm system to alert the individual and their support systems when blood glucose levels are too low.”
Living with Type 1 Diabetes in the Workplace
The mental load and time commitment required to monitor symptoms and blood sugar levels closely, or reminding a loved one to do so, has an impact on the workplace. This mental load impacts not only the employee with Type 1 diabetes, but also the spouse, mother or father of someone with type 1 diabetes.
Some individuals have a form of Type 1 diabetes that makes it hard to notice the physical symptoms of low/high blood sugar. Even those who can detect the signs and symptoms more easily worry that signs and symptoms will be missed while sleeping – with severe consequences.
Worrying leads to poor quality sleep, which impacts alertness, mood and productivity during the day. The parent or spouse of someone with Type 1 diabetes is also worried and anxious, making them less focused while at work.
We know that knowledge is power. If someone living with Type 1 diabetes and their family have access to real-time knowledge about their blood sugar levels, they can gain considerable freedom and control within their day-to-day life that improves productivity at work for everyone.
COVID-19 has presented an opportunity for policy makers, insurance companies and employers to make virtual care more integrated in the future. “We need to invest in the infrastructure needed to maximize virtual care. A lot of people, I think, are appreciating now that they don’t always have to come in to see their doctor, and that they can do a lot of this remotely,” says Dr. Simone. Less time at the doctor’s office means more time for other activities, including more time engaged at work.
Employee Journey: John Whitehead, Niagara Casinos
John Whitehead is a bartender and server at Niagara Casinos. John has Type 1 diabetes and ignored it for years. When John finally decided to better manage his disease, he was using an insulin pump and monitoring his blood sugar and food intake constantly throughout the day.
When John initially decided to get a continuous glucose monitor to help regulate his insulin and alert him to regulate his dose, he realized both his work benefit plan and the public system didn’t cover the device.
John and another colleague, the mother of a child with Type 1 Diabetes, were able to show how important the device would be to their day-to-day lives and gained access to the device through their employer.
John estimates that his monitor has saved him dozens of trips to the hospital and positively impacted his workplace. Before he had the monitor, John was checking his blood sugar levels about 10 times per day – and now – “I haven’t had a single low blood sugar event that required help from my coworkers, which was frequent before.”
“Not only has my workplace been impacted, my home life has improved. Better management of my blood sugar has led to better mood and I can go to bed without worrying that I won’t wake up, which had become a problem.”
John’s story highlights the need for access to the right tools in order to keep individuals and workplaces at their best. bh


Virtual care as a model for the future
Virtual care has become a critical health tool during COVID-19. Half of Canadians have accessed some form of virtual care with high levels of satisfaction, according to a poll conducted by the Canadian Medical Association (CMA) in May.3
Benefits of virtual care reported by Canadians include decreased costs, improved access to specialists and quicker access to test results. For Type 1 diabetes care, integrated sensors and virtual care could reduce the need for in-person medical visits dramatically.
Beyond COVID-19, the CMA has committed to build on the recent momentum and anticipates a growing demand for virtual care among Canadians. And why not? It is easy to see the convenience, comfort and quality that virtual care can provide. In fact, the CMA poll revealed that 38% of Canadians would choose virtual care over an in-person doctor’s visit in the future.
For those living with Type 1 diabetes, greater use of integrated sensors and virtual care will mean:
- Greater freedom, with care accessible from anywhere at anytime
- Increased support from medical professionals and family. The ability to transmit data to clinics and family means some of the burden is shared.
- Greater productivity at work. Decreased worry and mental load associated with monitoring blood sugar, more restful sleep, fewer absences and greater presenteeism.
- Less time away from work and other activities for medical visits.
With access to virtual care and supporting technologies, it is now possible to support a greater number of employees and their health. In bh 16(2), we highlighted the concept of workforce sustainability – which includes ensuring an adaptive workforce and one that is inclusive, diverse and supports the health and safety of employees.
Keeping employees like John Whitehead, and others like him, productive and in the workforce contributes to workforce sustainability. This is good for society and business.
References and Sources for information on Type 1 diabetes:
1Diabetes Canada
2Diatribe.org
3CMA, https://www.cma.ca/sites/default/files/pdf/virtual-care/cma-virtual-care-public-poll-june-2020-e.pdf
In partnership with DEXCOM
![]()

